What is RCT
RCT an acronym for Root Canal treatment, also known as Root Fillings or Root Treatment, is a dental procedure that is performed to try and save a tooth that is at risk of being lost.
Structure of your tooth.
All teeth are formed by Enamel, Dentin and Pulp. The Enamel is the first layer of the tooth, it is the hardest tissue that covers the crown, the part of the tooth that you see in your mouth.
The Dentin is the second layer, softer than enamel, and protect the pulp.
The Pulp Cavity is the centre of the tooth formed of nerves, blood vessels and cells, which expand into the Root Canals, giving the tooth hot and cold sensations and keeps the tooth alive.

When and how RCT is performed.
RCT is performed usually when the tooth is affected by an infection of the pulp, this can occur due to a trauma, deep cavity, and abscess at the apex (tip of the root). To confirm the reason of the pain the dentist will take and X-ray of the tooth and check if a root canal treatment is necessary. The other reasons for root canal procedure can be for elective cosmetic dentistry treatments. This can occur as an unwanted side effect of having veneers or crowns. The risk of this occurring for veneers is LESS THAN 5% and for crowns it is up to 20%. This is according to the prevailing dental research currently available. An experienced cosmetic dentist in London like Marylebone Smile Clinic can asses your teeth health and provide you with the best options available.

Root Canal Treatments are often performed by an Endodontist, which is a specialist dentist trained in treatment of the pulp. They can also be performed by general dentists, and approximately 90% of all RCTs are done by local dentists. Endodontists classically manage extreme and challenging root canal treatments, but they also can be expected to have a higher success rate with ordinary root treatments.
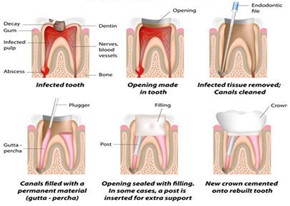
A Root canal Treatment procedure is divided into six steps:
- Access: The tooth is opened from the top of the crown and the decay is cleaned to reach the pulp.
- Disinfection: The infected tissue is removed from the root canals with specific instruments called endodontic files.
- Root Filling: After being cleaned the canals are filled with a permanent material called Gutta-percha or GP point.
- Top Filling: When the canals are filled the part of tooth that has been opened to access the canals is closed with a filling material (same used to complete a normal filling procedure).
- Protection: Due to the root canal treatment the tooth is more brittle and not strong as before and needs to be protected by a crown or onlay, so an impression is taken and send to the Dental Technician.
- Fitment: After 1-2 weeks the permanent crown will be fitted, usually with a neutral and low toxicity cement.
What Equipment is used to perform a root canal treatment?
Rubber dam instruments: used to isolate the tooth during the procedure, rubber dam, rubber dam punch, rubber dam clamp forceps, rubber dam frame and teeth clamp (Molar clamp, premolar clap and incisor or butterfly clamp).
Metal ruler: used with a file to measure the length of each root canal.
Apex locater: a machine that is used to determine the working length of the canals.
Gates Glidden drill: used to access each root canal by drilling the base of the pulp chamber.
Barbed broach: hand or rotary, used to remove (extirpate) any pulp tissue.
Reamer: used to enlarge the root canals down to the root apex.
Endodontic file: they can be hand or rotary files used to smooth the canals walls and remove any debris. ProTaper gold are the most used and is made of nickel-titanium. This is an alloy developed out of the need for a machinable metal that can withstand high levels of torque and stress before breaking. Thankfully, Ni-Ti has excellent properties and is unlikely to break. Older materials such as stainless streel is more likely to separate and or that reason it is used in some isolated scenarios.
Irrigation syringe: chlorhexidine, sodium hypochlorite peroxide (concentration 0.5-5%) used to disinfect and wash out any debris from the root canals.
Paper point: used to dry the canals.
Gutta Percha point: used with a canal cement (zinc oxide-eugenol) to seal the canal.

What happens after a Root Canal Treatment?
After the root canal treatment, because the pulp of the tooth has been removed and replace with a filling material, the tooth is not vital anymore and loose sensation from that specific tooth. This means that you will not be able to feel any hot or cold sensation. If not covered with crown or onlay, the tooth can appear darker than the rest of the teeth, this is due form the dehydration of the dentin. You can try and improve the colour with internal tooth bleaching that is performed from the dentist by making a small hole on the tooth surface that allowed the whitening gel product to enter the tooth.
How is sensation changed, how does it look, can I eat normally, does it require maintenance, what to do if I get problems after?
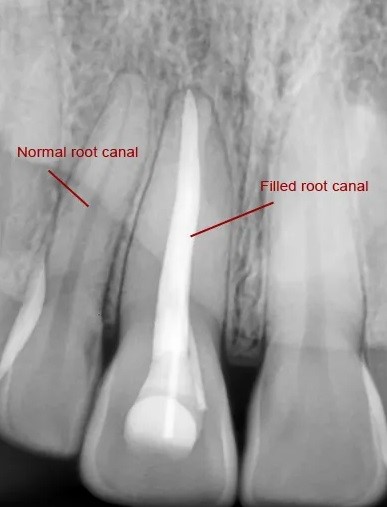
How to Look at your Teeth X-rays

These 3 X-rays are divided into before treatment, after treatment and healing at 12 months:
Before treatment: before the root canal treatment is performed on the x-ray you can see a black shadow in between the two roots of the tooth. This is the sign of the infection that is causing the pain.
After treatment: after the procedure is completed on the x-ray you can see two white lines inside the tooth roots, this is the root filling material placed after the infected pulp has been removed. You can also see that the black shadow between the roots is still there, and this is because it will take some time before the infection is completely healed.
Healing at 12 months: in this x-ray, taken 12 months after the root canal treatment, you can clearly see that the black shadow in between the roots of tooth is nicely healed.
Does an RCT tooth need protection after the treatment?
It is recommended to have a crown or onlay after root canal treatment to provide resistance from lateral forces. After RCT the tooth is not strong as before and it has a higher chance of fracture if not protected.
What are the risks?
- GP placed beyond apex, the gutta percha is too long compared to the root canal.
- GP not filled to base of canal, the gutta percha is too short compared to the root canal.
- 2nd/3rd attempts lower success rate. If the first attempt is not successful, the dentist can try and reperform the procedure, but the risk of failure is higher at every subsequent attempt.
- Fracture – fracture lines are not always visible on x-ray and sometimes the dentist only confirms when the tooth is accessed. In the case of a vertical fracture the only option is to remove the tooth. There is a risk of fracture after the root canal procedure is completed if the tooth is not protected with a crown or onlay as the tooth is not strong enough. These are often lateral or oblique fractures that are problematic but less catastrophic for a tooth.
- Failure of coronal seal, this can happen if the crown or onlay is not fitting well or if the area has been contaminated with saliva.
- Pain – it is normal to feel some pain and discomfort after a root canal procedure. The dentist will recommend taking pain relievers such as paracetamol and ibuprofen.
- Paraesthesia can occur after the procedure if the dental nerve has been irritated or damaged. When the local anaesthetic wears off, you will feel a change in sensation that will not subside if the nerve has been damaged.
- Fractured files – Endodontic files are very thin instruments and sometimes can separate during the root canal procedure. These files are exceedingly difficult to remove, and the dentist can try to remove it by using ultrasonic instrument or surgically. The more likely option is to leave it in the root canal and complete the procedure. Your dentist would explain this to you during or after the procedure.
- Extrusion of sodium hypochlorite, chlorhexidine (concentration 0.5-5%, often 3%) are used during the procedure to disinfect and wash out any debris from the root canals with an irrigation syringe. One of the risks is to extrude it beyond the apex which can be painful and can cause swelling. The remedy for this initially is to use local anaesthetic to attempt to neutralise the alkali solution and provide pain relief until medical advice can be sought.
FAQs
How do I know if I need RCT?
Those are common signs that a root canal is needed:
- If you have severe pain form the tooth when chewing or putting pressure on the tooth. If it is spontaneous and does not respond to pain killers, this is a sign the nerve is deteriorating.
- Sensitivity or pain form hot or cold temperatures that lasts longer than 2 minutes
- If you had a trauma and you experiencing pain, or the tooth has discoloured.
- If the gum around the tooth is swollen and tender and the side of your face and check is affected.
Is RCT painful?
No, root canal treatment is not painful. Before starting the procedure, the dentist will administer local anaesthetic and will make sure that the tooth is numb, and you do not feel any pain. After the procedure it is possible to feel discomfort from the treated area, in this case the dentist will advise to take pain relief (ibuprofen, paracetamol).
Do I need a crown after a root canal?
The dentist will advise to have a crown or onlay after the root canal treatment as the tooth is more brittle and the risk of fracture is higher than a normal tooth.
How soon after a root canal should I have a crown?
After completing the root canal procedure, the dentist will take an impression of the tooth and send it to the Dental Technician. Usually, the final crown or onlay is ready to be fitted after one-two weeks. It is important to have the crown or onlay placed within four weeks of completion of the root canal treatment.
How long does a root canal treatment last?
A successful root canal treatment can last ten years or longer.
Is RCT done in one visit?
Usually, the root canal treatment is performed in one visit but sometimes can be done in two or more visits, specifically if the patient has trouble keeping the mouth open for long time.
Can RCTs fail?
Yes, a root canal treatment can fail. The most common reason for a RCT to fail is secondary infection. This is the same tooth becoming reinfected due to an inadequate seal on the tooth or improper treatment at the first instance. The probability of this occurring is approximately 20% across all RCTs placed in the UK. The success rate is higher with specialist root canal dentists.
Is RCT expensive?
Root canal treatment performed by an Endodontist is priced between £600 and £1500.
Root canal treatment performed by a general dentist can be between £300 and £700, plus the crown or onlay cost.
On the NHS, an RCT and crown falls under a Band 3, price at £282.80.
What is better, extraction or RCT?
This is case dependant and specific to your preferences and circumstances. The factors to consider are how much tooth structure remains, the position of the tooth in the mouth according to aesthetics and function. It is best to discuss this with your dentist as there is no correct answer for all situations.
What happens if a file fractures in my tooth?
If a file fractures inside the root canal during the procedure, the dentist will try and remove it but, if this is not possible the options are to leave the file and complete the root canal procedure or attempt removal. Depending on the location of the separate piece, your dentist will make a judgment based on the likelihood of retrieval against the risk of damage to the tooth.
Want to know more?
Get in touch to enquire about our services or to book an appointment.


